Lights, Clips, Powders, Heat, Action: Finding and Stopping GI Bleeds
Summary: Olympus’ Marketing Director of Core GI EndoTherapy Christian Stroupe, and Senior Manager of Core GI Procedures Robert Barrett, discuss the Olympus® hemostasis portfolio. They cover the company’s developments from endoscopic bleed detection using imaging technology in the EVIS X1™ endoscopy system to treatments with specially designed clips, sprays, and thermal therapy.
Many gastrointestinal bleeds are minor and may resolve on their own. But when they don’t, especially during a procedure, things can get stressful, according to Robert Barrett, Senior Manager of Core GI Procedures for Olympus. Barrett, who oversees a product that supports detecting the source of such bleeds, was a guest on DeviceTalks’ OlympusTalks podcast, along with Christian Stroupe, Marketing Director of Core GI EndoTherapy at Olympus, who discussed the wide range of GI bleeds, and Olympus’ growing portfolio of therapeutic endoscopic devices and graspers.
GI Bleeds at a Glance
GI bleeds are categorized as either upper or lower bleeds. Stroupe said that upper GI bleeds—spanning from the mouth through the small intestine—are more common, accounting for roughly 70% of GI bleeding.1 Upper GI bleeding can be caused by overuse of NSAIDS, anticoagulants, or medical conditions such as peptic ulcers or gastritis, for example.1,2 Lower GI bleeds, which occur in the large intestine, can be related to conditions such as diverticulosis, colitis, or cancer, for example, or can be procedure-related.1
Overall, the incidence of GI bleeds is dropping,1 but for severe cases, the impact can be substantial. For upper GI bleeds, “the mortality rate is between 6 to 10%,” said Barrett. Lower GI bleeds have a 2 to 4% mortality rate. “This comes with a significant economic burden” to the tune of $2.5 billion in U.S. healthcare costs, based on research he cited.2
Stroupe said endoscopic procedures are often performed to treat GI bleeding, which is consistent with American Society of Gastrointestinal Endoscopy guidelines published on GI bleeding topics over the years.3
Hear Stroupe discuss the procedures associated with GI bleeding, and the settings where the Olympus® hemostatic portfolio can be used.
‘You Just See Red Everywhere’
“One of the key points is always to find the bleed; identify where the bleed is coming from,” stressed Barrett. In the case of substantial bleeds, he noted that flushing pumps and suction can temporarily remove blood, but visualization can quickly diminish as bleeding continues, even while using white light endoscopy. “Perhaps you have a pool of blood, or the blood’s coming out at the endoscope and you’re not able to see clearly, that’s when it becomes a challenge, because you just see red everywhere, and you don’t know: Is it coming from the left, is it coming from the right?”
Three Wavelengths of Light
“One of the technologies we have on our EVIS X1™ endoscopy system is called Red Dichromatic Imaging [RDITM technology],” he explained. “The way [RDI technology] works is it makes use of an amber LED that’s unique to the CV-1500 video processor,” that’s part of the EVIS X1 endoscopy system, Barrett explained. “The technology uses three wavelengths of light: green, amber and red,” he said. “It passes through a filter because we want very specific narrow bands of light for this to work effectively,” he adds. “The amber light is highly absorbed by blood, so … the highest concentration is at the bleed point. Everything else surrounding [this point] is more dilute. The bleeding point appears darker than the surrounding areas and therefore is more visible,” Barrett explains. “That’s how you know … where the bleed is.”4
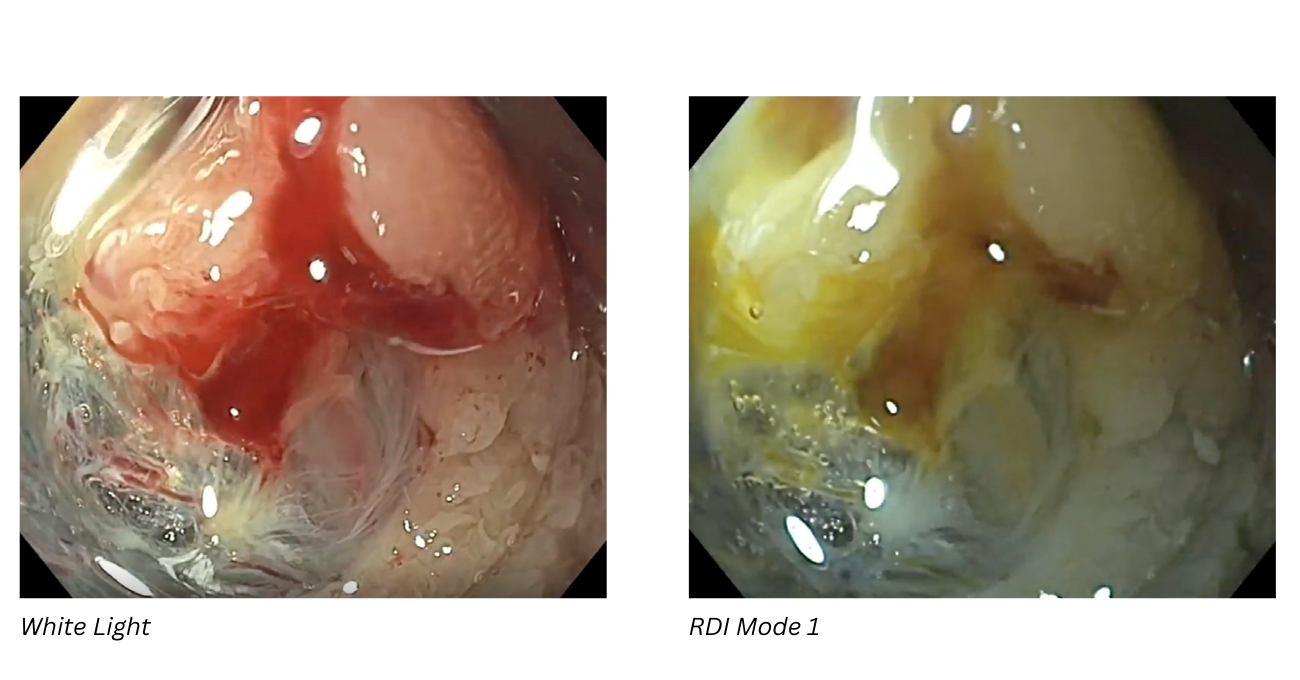
Images provided by Dr. Gregory Haber using a GIF-HQ190 gastroscope.
Listen to Barrett discuss how RDITM technology can be used proactively to view vessels before a procedure.
Watch the Clip
“Once we find the bleed through something like RDI™ [technology], it depends on the type of bleed, obviously, but many times physicians are looking to do something with mechanical hemostasis,” said Stroupe. In such cases, “we’re using clips, hemostatic clips,” with the idea of “capturing [the] bleeding point with a mechanical force … that closes the bleed … and achieves hemostasis.” Olympus’ most recent addition to its clip (a.k.a. mechanical therapy) portfolio is the single-use Retentia™ HemoClip manufactured by Yangzhou Fartley Medical Instrument Technology Co., Ltd. with availability announced in March 2025.
Powder Power
Still, GI bleed cases can prove tricky. “Maybe they’ve identified where that bleeding point is … but it’s a little more challenging to get to” because of the scope position, Stroupe suggested. The EndoClot® PHS is a powder-based hemostatic agent manufactured by EndoClot Plus Co., Ltd. that is applied endoscopically through a catheter, he explained. Deployment of the powder involves an air compressor outside of the scope. “The physician will pass a hollow tube catheter through the scope channel. Once they’ve identified where they want to put [the powder] on, they literally turn the compressor on and start applying powder,” said Stroupe. Sometimes called painting, he added, “They’ll spray across … the mucosal area and hit not only the bleeding point, but sometimes all around it.”
Getting a Grasp on It
Some GI bleeds may benefit from targeted monopolar coagulation, Stroupe explained. The Coagrasper™ Hemostatic Forceps is similar to a hot biopsy forcep, which is connected to an electrosurgical generator. When activated, it delivers a controlled electric current, which heats the tissue in a focused manner. “It allows you to … grasp the vessel and pull it back [to avoid] thermal damage to the rest of the mucosa” because the vessel is isolated in the forceps. The device is primarily used for interventional cases such as endoscopic submucosal dissection or endoscopic mucosal resection, he said.
Overall, the more tools physicians have in the hemostasis toolbox the better, given the serious morbidity and mortality consequences, and the significant financial burden.2 The good news is that GI bleed rates are dropping,1 as clinical guidelines continue to fine tune recommended interventions, and companies like Olympus continue to add to that toolbox by developing endoscopic technologies to help find—and stop—GI bleeds.
The EVIS X1™ endoscopy system is not designed for cardiac applications. Other combinations of equipment may cause ventricular fibrillation or seriously affect the cardiac function of the patient. Improper use of endoscopes may result in patient injury, infection, bleeding, and/or perforation. Complete indications, contraindications, warnings, and cautions are available in the Instructions for Use (IFU).
RDI™ technology is not intended to replace histopathological sampling as a means of diagnosis.
RDI is a trademark of Olympus Corporation, Olympus America, Inc., and/or their affiliates.
Performing hemostasis within the GI tract is a technically demanding procedure and use of hemostatic clips and associated devices may result in patient injury including but not limited to inflammatory reaction, infection, bleeding and perforation.
Performing hemostasis within the GI tract is a technically demanding procedure and use of EndoClot PHS and associated devices may result in patient injury including but not limited to inflammatory reaction, bowel rupture and air embolism.
References
1. DiGregorio AM, Alvey H. Gastrointestinal Bleeding. [Updated 2023 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537291/
2. Parker DR, Luo X, Jalbert JJ, Assaf AR. Impact of upper and lower gastrointestinal blood loss on healthcare utilization and costs: a systematic review. J Med Econ. 2011;14(3):279-87.
3. ASGE.org. ASGE Guidelines. Accessed August 7, 2025. https://www.asge.org/home/resources/publications/guidelines#newly-published
4. Data on file with Olympus (DC00489968).