Laparoscopic Option for Live Liver Donations Offers Donor Benefits
Medical dramas play out in real life every day. As of May 2022, more than 11,200 individuals are on the U.S. liver transplant waiting list, but just over 10,000 liver transplants are done each year.1 To bridge this gap, live liver donations in the U.S. have steadily increased in recent years to an all-time high of 568 in 2021.2 Living donors can donate a portion of their liver, the only human organ able to regenerate itself.3 A laparoscopic technique to surgically resect the donor liver (hepatectomy) may offer a quicker recovery with less scarring and other benefits associated with minimally invasive procedures.4
Living donor liver candidates
In the U.S., liver transplant candidates are prioritized based on their Model for End-stage Liver Disease (MELD) score, a system used by the United Network for Organ Sharing, a division of the U.S. Department of Health and Human Services. The higher the MELD score, the sicker the patient, thus high scores receive top priority for deceased donor livers. These patients are not considered to be good candidates for living donors.5
Appropriate living donor candidates tend to have lower MELD scores. For example, certain patients with significant encephalopathy, or patients with smaller sized hepatic tumors who may have been recommended for transplant, could have MELD scores that do not qualify as high priority on the deceased donor list. These are examples of appropriate patient candidates for a living donor transplant.5
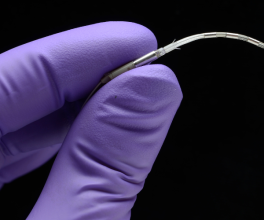
An alternative to open procedures
Living donor hepatectomies in the U.S. have typically been performed as open procedures, but mortality rates and complications of right lobe grafts have created a barrier to donation in some centers.6 In the early 2000s a few transplant centers began performing left-lateral sectionectomies for graft procurement in infants, opening the door of possibility for a minimally invasive adult donor hepatectomy.6
The first fully laparoscopic adult donor/recipient case in the U.S. was reported in September 2015 in New York City at New York-Presbyterian/Columbia University Medical Center.7 A surgical team led by Benjamin Samstein, MD, published their findings on the benefits of a fully laparoscopic left-sided donor hepatectomy compared to open and hybrid approaches, observing that donors who underwent the fully laparoscopic approach spent fewer days in the hospital and returned to work sooner.6
In August 2019, Cleveland Clinic published details on its first fully laparoscopic adult donor hepatectomy. Choon Hyuck David Kwon, MD, PhD, and his team performed the successful laparoscopic living donor hepatectomy for liver transplant. The donor was a 29-year-old male who was not a blood relative of the 66-year-old male recipient. Dr. Kwon previously founded a laparoscopic living donor surgery program at Samsung Medical Center in South Korea, where the procedure is done more frequently.8
Hurdles to U.S. adoption
“[Living donor hepatectomy liver transplant] is one of the most complex surgeries that can be done laparoscopically,” Dr. Kwon said in the article posted on the Cleveland Clinic site. In the U.S., laparoscopic surgery and liver transplant are two separate disciplines and few pursue both, he observed. To get a program up and running, “You need to practice daily,” Dr. Kwon said. “The whole team needs to be used to the setting,” including surgical instrument placement and teamwork during complex laparoscopic liver procedures. In addition to an extensive learning curve and dual-specialty surgical expertise, Dr. Kwon observed skepticism among U.S. transplant surgeons about adoption due to larger-sized American patients, compared to the Asian populations in which this is more common. He expressed hope that continued successful transplants in centers like his will dispel this notion.8
Additional Resources
Since the first Cleveland Clinic case, Dr. Kwon discusses how the program has expanded in this Cleveland Clinic podcast.
Read more about hepatic resections or watch videos on the Laparoscopic/Open HPB Surgery page, under the General Surgery page in the Olympus On-Demand Library.
Dr. Kwon reported receiving grant(s) from Olympus.
References
1. U.S. Department of Health and Human Services. Organ Procurement and Transplantation Network. Data - OPTN (hrsa.gov) Accessed May 17, 2022.
2. U.S. Department of Health and Human Services. Organ Procurement and Transplantation Network. National data - OPTN (hrsa.gov) (Category: Transplant, Organ: Liver, Transplants by donor type, All donor types 2021=10,109, Living Donors 2021=568) Accessed May 18, 2022.
3. American Liver Foundation. Living Donor Liver Transplant – An Introduction for Donors and Recipients — American Liver Foundation. Accessed May 17, 2022.
4. Gao Y, Wu W, Liu C, Liu T, Xiao H. Comparison of laparoscopic and open living donor hepatectomy: A meta-analysis. Medicine (Baltimore). 2021;100(32):e26708.
5. Brown RS Jr. Pros and cons of living donor liver transplant. Gastroenterol Hepatol (N Y). 2008;4(9):622-624.
6. Samstein B, Griesemer A, Cherqui D, et al. Fully laparoscopic left-sided donor hepatectomy is safe and associated with shorter hospital stay and earlier return to work: A comparative study. Liver Transpl. 2015;21(6):768-773.
7. Columbia Surgery, New York Presbyterian. Laparoscopic Living Donor Hepatectomy at Columbia | Columbia Surgery. Accessed May 17, 2022.
8. Cleveland Clinic, Consult QD. First Purely Laparoscopic Living Donor Hepatectomy for Liver Transplant is a Landmark for Cleveland Clinic – Consult QD. Accessed May 17, 2022.