Raising Awareness & Lowering Barriers to Lung Cancer Screenings
It’s been eight years since the U.S. Preventive Services Task Force first released its guidelines for annual lung cancer screenings, but screening rates among at-risk adults remain low. Currently, the national screening rate for those considered at high risk is only 5.7 percent.1
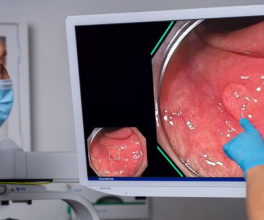
Last year, the United States Preventive Service Task Force (USPSTF) updated its guidelines for annual screenings using low-dose computed tomography (LDCT), recommending screenings for adults ages 50 to 80 who have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years.2 The recommendation had previously been 30 pack-years for ages 55 to 80.
Education of both patients and primary care physicians remain key issues in raising lung cancer screening rates along with lowering barriers for patients such as simplifying the shared-decision making process, according to some doctors.
Educating Primary Care Physicians
Dr. Stephenie Kennedy-Rea is the associate center director of the West Virginia University Cancer Institute and spoke last fall during a webinar about establishing the institute’s new mobile lung cancer screening unit.
Lung cancer accounts for about 18% of all new cancer cases in the state and kills more people in West Virginia annually than breast, colorectal, prostate, and cervical cancers combined3, according to Kennedy-Rea. More than 200,000 people in the state are eligible for lung cancer screenings but less than 4% have received screenings4, she said, noting the entire state has 26 American College of Radiology accredited screening facilities.
Before launching the mobile screening facility, the institute surveyed and interviewed doctors in the state and learned that most primary care physicians didn’t understand the screening guidelines and the shared decision-making process, Kennedy-Rea said.
During the shared decision-making process, physicians and patients work together to make decisions and select tests, treatments and care plans that balance risks and expected outcomes with patient preferences.
The survey also revealed that primary care physicians didn’t understand whether screenings were covered by insurance and the insurance codes for such procedures, Kennedy-Rea said. As a result, they weren’t referring patients for screenings.
“Primary care physicians are the gatekeepers to lung cancer screenings, really to all cancer screenings,” Kennedy-Rea said.
The institute completed a community survey that was used to develop patient education cards distributed to providers, she said.
“Primary care physicians are the gatekeepers to lung cancer screenings, really to all cancer screenings.”
Lowering Barriers
Dr. Gerard Criner is the chair and a professor of thoracic medicine and surgery at the Lewis Katz School of Medicine at Temple University and director of the Temple Lung Center.
Criner said during an interview about Lung Cancer Awareness Month5 that the earlier guidelines were limited in that studies failed to recruit women and minorities, so they were based on data that didn’t incorporate those groups for whom the cancer risk can be greater with a lower-volume smoking history.6 And while he’s hopeful the new guidelines will increase the screening numbers, he said one of the primary barriers to increased screening rates is a cumbersome shared decision-making process for patients.
Unlike other screenings, a primary care physician must have a face-to-face consultation with a patient ahead of ordering a low-dose CT scan for lung cancer, for instance, which must be documented before the Centers for Medicare and Medicaid Services (CMS) will approve the scan, he said.
The process can be even more cumbersome for older patients, some of whom may be on supplemental oxygen and need assistance getting to and from appointments, he said.
“If they can come in and get a test, that’s easy,” Criner said. “If they have to come in and get an office visit first to do shared decision making before the order can get in … that’s another element of an obstacle to them.”
During the COVID pandemic, telehealth visits were allowed for shared decision-making, a change Criner would like to see made permanent.
But some of the discussion points that go into shared decision-making aren’t even germane to the lung-cancer screening and could instead be discussed between doctor and patient in the event treatment is necessary, Criner said. He advocates streamlining the process by developing an easily understandable, scripted communication made available to patients in writing or via video before undergoing a scan, he said.
In order to better facilitate and manage lung cancer screenings, Criner points to the creation of centers of excellence. A larger health system could employ a spoke-and-hub approach in which the “mother ship” would house the centralized infrastructure and primary care physicians administer screenings. That data is then fed into the central hub, where navigators monitor results and direct patients, as needed, to pulmonary specialists, Criner said.
Changing policy surrounding shared decision-making and screenings is a heavy lift, so Criner strongly advocates for increased public outreach and education.
“To be honest, I think most of the public doesn't even know this exists,” he said of lung cancer screening recommendations.
It would seem that, as with many technologies, the “if they build it, they will come,” mentality is not working with lung cancer screening. More simplicity to the decision-making process, as well as awareness-building with patients and primary care physicians, may one day turn the tide, which will mean a more hopeful outlook for lung cancer patients.
1 American Lung Association, State of the Lung Cancer 2020 Report, Accessed August 2021
2 https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
3 American Cancer Society, Cancer Statistics Center, Accessed December 2021, https://cancerstatisticscenter.cancer.org/
4 American Lung Association, State of the Lung Cancer 2020 Report, Accessed December 2021, https://www.lung.org/research/state-of-lung-cancer/states/west-virginia
5 Sept. 17, 2021, interview with Dr. Gerald Criner
6 Rivera, MP et al. “Addressing Disparities in Lung Cancer Screening Eligibility and Healthcare Access. An Official American Thoracic Society Statement.” American Journal of Respiratory and Critical Care Medicine. Published Oct. 1, 2020.